Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting many women of reproductive age. While it can cause various symptoms like irregular periods and fertility challenges, one of the most visible and often distressing manifestations is acne. PCOS-related acne tends to be persistent, inflammatory, and resistant to typical over-the-counter treatments. While medical management is often essential for PCOS, there’s growing interest in natural strategies involving diet, lifestyle, and specific supplements that may help support skin health and manage acne symptoms alongside conventional care.
This article explores the typical symptoms of PCOS acne, why it occurs, and evidence-based natural approaches that may offer complementary benefits.
Important Disclaimer: PCOS is a medical condition that requires proper diagnosis and management by healthcare professionals (like an OB/GYN, endocrinologist, or primary care physician). The natural strategies discussed here should be considered complementary to, not replacements for, medical advice and prescribed treatments. Always consult your doctor before making significant dietary changes or starting new supplements, especially when managing a condition like PCOS.
Understanding PCOS and its Link to Acne
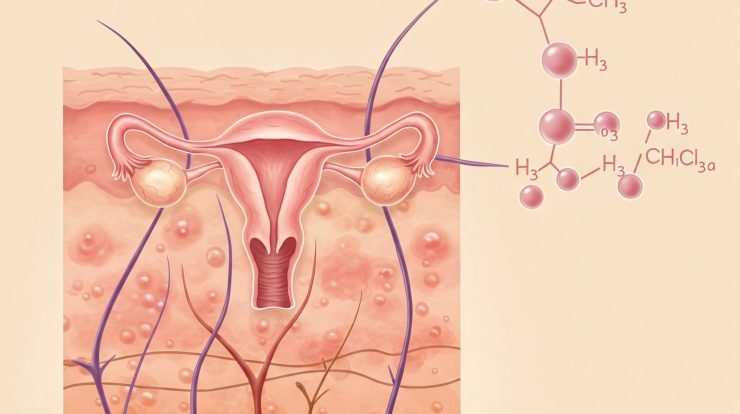
PCOS is characterized by hormonal imbalances, primarily involving:
- Hyperandrogenism: Elevated levels of androgens (“male” hormones like testosterone, which women also produce). Androgens directly stimulate the skin’s sebaceous (oil) glands, leading to increased sebum production – a key factor in acne development.
- Insulin Resistance: Many women with PCOS also have insulin resistance, where the body’s cells don’t respond properly to insulin. This leads the pancreas to produce more insulin (hyperinsulinemia). High insulin levels can further increase androgen production by the ovaries and may also directly stimulate oil glands and inflammation.
This combination of excess androgens and often elevated insulin creates a perfect storm for developing persistent and inflammatory acne.
Typical PCOS Acne Symptoms:
- Location: Often concentrated on the lower face – jawline, chin, neck, and sometimes upper back or chest.
- Type: Tends to be inflammatory (red, painful papules, pustules) and often includes deeper, tender cysts or nodules. Comedones (blackheads/whiteheads) may also be present.
- Persistence: Often stubborn, lasting beyond teenage years into adulthood.
- Cyclical Flaring: May worsen around menstrual periods.
- Resistance to Standard Treatments: Often doesn’t respond well solely to typical OTC acne washes or spot treatments.
Natural Treatment Approaches for PCOS Acne (Complementary Strategies)
These approaches aim to address underlying factors like insulin resistance and inflammation or soothe symptoms:
1. Dietary Strategies
Diet plays a crucial role in managing PCOS symptoms, including insulin resistance and inflammation.
- Low Glycemic (Low GI) Diet:
- Why: This is often a primary dietary recommendation for PCOS. Low GI foods cause a slower, lower rise in blood sugar and insulin levels. By reducing insulin spikes, this diet may help lower androgen production and reduce IGF-1 levels, potentially decreasing sebum production and inflammation.
- Focus: Emphasizes whole grains (oats, quinoa, brown rice), legumes (beans, lentils), non-starchy vegetables, most fruits, lean proteins, and healthy fats. Limit refined carbohydrates (white bread/rice/pasta), sugary drinks, sweets, and processed foods.
- Anti-Inflammatory Diet:
- Why: PCOS is associated with chronic low-grade inflammation, which can worsen acne. An anti-inflammatory diet focuses on foods that combat inflammation.
- Focus: Rich in omega-3 fatty acids (salmon, mackerel, flaxseeds, chia seeds, walnuts), antioxidants (berries, leafy greens, colorful vegetables, green tea), nuts, seeds, olive oil, and spices like turmeric. Limit processed foods, trans fats, excessive omega-6 fats (often found in processed vegetable oils), and potentially refined sugars.
- Dairy Consideration (Individualized):
- Why: As discussed in general acne research, some studies link milk intake (especially skim) to acne, possibly via IGF-1 pathways relevant to PCOS.
- Approach: This is highly individual. Some women with PCOS find reducing or eliminating dairy helpful, while others see no difference. If considered, a strict elimination trial (4-8 weeks) followed by careful reintroduction is necessary to assess personal sensitivity. Ensure adequate calcium/Vitamin D from other sources if eliminating dairy long-term (consult a dietitian/doctor).
2. Lifestyle Modifications
- Regular Exercise: Crucial for improving insulin sensitivity, managing weight (if applicable), and reducing stress. Aim for a combination of aerobic exercise and strength training. Even moderate activity is beneficial.
- Stress Management: Chronic stress negatively impacts hormones and inflammation. Incorporate stress-reducing techniques like yoga, meditation, deep breathing exercises, mindfulness, spending time in nature, or engaging in hobbies. Prioritize adequate sleep (7-9 hours).
- Weight Management (If Applicable): For women with PCOS who are overweight or obese, even modest weight loss (5-10% of body weight) can significantly improve insulin resistance, lower androgen levels, regulate periods, and potentially improve acne.
3. Specific Supplements (Use with Caution and Medical Guidance)
Certain supplements have shown promise specifically for PCOS symptoms, which may indirectly benefit acne. Always consult your doctor before starting any supplements.
- Inositol (Myo-inositol & D-chiro-inositol):
- Why: These are vitamin-like compounds involved in insulin signaling. Numerous studies suggest inositol supplementation (often in a specific ratio, typically 40:1 Myo- to D-chiro) can improve insulin sensitivity, regulate menstrual cycles, and reduce androgen levels in women with PCOS. Improvement in acne has been noted as a secondary outcome in some studies. Often considered one of the most evidence-supported natural supplements for PCOS.
- Spearmint Tea:
- Why: Some small studies in women with PCOS suggest drinking two cups of spearmint tea daily may have mild anti-androgenic effects, potentially reducing free testosterone levels.
- Caveat: Direct evidence for significant acne improvement is limited; effects are likely modest if present.
- Zinc:
- Why: Plays roles in skin health, wound healing, and inflammation. Some studies link lower zinc levels to acne severity. Supplementation may help reduce inflammation.
- Caveat: Dosage is important; excessive zinc can have side effects. Consult your doctor.
- Omega-3 Fatty Acids:
- Why: Potent anti-inflammatory effects. Supplements (fish oil, algal oil) can help if dietary intake is insufficient.
- Vitamin D:
- Why: Deficiency is common in women with PCOS and linked to insulin resistance, inflammation, and hormonal imbalances.
- Action: Get levels checked by a doctor and supplement only if deficient under their guidance.
What Natural Treatments Cannot Do
It’s vital to maintain realistic expectations:
- Natural approaches cannot cure PCOS.
- They are unlikely to completely eliminate moderate-to-severe hormonal acne on their own.
- They do not replace necessary medical treatments like Metformin (for insulin resistance), hormonal contraceptives, or anti-androgen medications (like Spironolactone) if prescribed by your doctor for managing PCOS or related severe acne.
Importance of Medical Diagnosis and Management
Self-diagnosing PCOS based on symptoms like acne can be inaccurate.
- Get Diagnosed: See a healthcare professional (OB/GYN, endocrinologist) for proper diagnosis based on the established Rotterdam criteria (usually requiring two out of three: irregular periods, signs of high androgens, polycystic ovaries on ultrasound).
- Work with Doctors: Collaborate with your doctors to manage the underlying PCOS. This often involves lifestyle changes and may include medication.
- See a Dermatologist: A dermatologist can provide targeted acne treatments (topical retinoids, antibiotics, benzoyl peroxide, etc.) that work alongside your PCOS management plan.
Conclusion
Acne is a frequent and often challenging symptom for women with Polycystic Ovary Syndrome, driven primarily by underlying hormonal imbalances (excess androgens) and frequently linked insulin resistance. While medical diagnosis and management by healthcare professionals are essential, natural strategies can play a significant complementary role. Focusing on a low-glycemic, anti-inflammatory diet, incorporating regular exercise, managing stress, and considering evidence-supported supplements like inositol may help improve insulin sensitivity, reduce inflammation, and potentially lessen the severity of PCOS-related acne for some individuals. Consistency and patience are key, and these natural approaches work best when integrated into a comprehensive management plan developed with your doctor, endocrinologist, and dermatologist.
