For many women, the arrival of their period often brings an unwelcome guest: an acne flare-up. Those predictable pimples popping up along the jawline, chin, or neck in the week or so leading up to or during menstruation are a common frustration. This pattern, often referred to as “period acne” or “cyclical acne,” is typically a form of hormonal acne, directly linked to the natural ebb and flow of hormones throughout the menstrual cycle. While completely eliminating these hormonal fluctuations isn’t possible, understanding why they happen and implementing targeted strategies can significantly help manage and reduce the severity of these breakouts. This article explores the connection and offers practical tips for managing acne around your cycle.
Why Do Breakouts Happen Around Your Period? (The Hormonal Connection)
Your skin, particularly the oil glands (sebaceous glands), is highly responsive to hormonal changes:
- Estrogen Dominance (First Half of Cycle): After your period, estrogen levels rise, generally keeping skin relatively clear and less oily for many.
- Progesterone Rises (After Ovulation): Following ovulation (mid-cycle), progesterone levels increase. Progesterone can potentially cause slight skin swelling and compression of pores, making them more likely to clog.
- Pre-Period Hormone Drop & Androgen Effects: In the week leading up to menstruation, both estrogen and progesterone levels decline significantly. While androgen levels (like testosterone) remain relatively constant throughout the month, this drop in female hormones allows the effects of androgens to become more pronounced. Androgens are known potent stimulators of sebaceous glands.
- Increased Sebum: The relative increase in androgen influence triggers higher sebum (oil) production.
- Inflammation: Hormonal shifts can also trigger inflammatory responses in the skin.
This combination increased oil production, potentially tighter pores, and heightened inflammation creates the perfect storm for developing inflammatory acne lesions, often appearing on the lower face where hormone-sensitive receptors are concentrated.
Strategies for Managing Menstrual Cycle Acne
While you can’t stop your hormonal cycle, you can implement strategies to mitigate its effects on your skin:
1. Maintain a Consistent Core Skincare Routine (All Month Long)
This is the foundation. Don’t wait for the breakout to happen; manage your skin consistently throughout the month.
- Gentle Cleanser: Wash your face twice daily (morning and night) and after sweating with a mild, non-comedogenic cleanser. Avoid harsh scrubbing.
- Non-Comedogenic Moisturizer: Keep your skin barrier healthy and hydrated, even if you feel oily. A compromised barrier can worsen inflammation. Choose oil-free, non-comedogenic formulas.
- Daily Sunscreen (SPF 30+): Essential year-round. Sun exposure can worsen post-inflammatory hyperpigmentation (dark spots) left by breakouts.
2. Incorporate Targeted Acne-Fighting Ingredients
Regular use of certain ingredients can help keep pores clear and manage bacteria/inflammation:
- Salicylic Acid (BHA): An oil-soluble exfoliant that penetrates pores to dissolve clogs. Use it regularly (2-4 times a week, depending on tolerance) in a cleanser, toner, or leave-on treatment. You might consider increasing frequency slightly in the week before your period if your skin tolerates it well.
- Benzoyl Peroxide (BPO): Kills acne-causing bacteria (C. acnes) and helps reduce inflammation. Excellent as a spot treatment for active pimples that emerge. Using a low-strength (2.5%-5%) BPO wash once or twice a week preventatively leading up to your period might help some, but be cautious of potential dryness and irritation (and fabric bleaching).
- Topical Retinoids: (Adapalene available OTC in some regions; Tretinoin etc. by prescription). These Vitamin A derivatives are highly effective for long-term acne management and prevention. They regulate skin cell turnover, prevent clogged pores (microcomedones), and have anti-inflammatory effects. Requires consistent nightly use over months to see results and needs dermatologist guidance for prescription forms. Sunscreen is mandatory when using retinoids.
- Niacinamide: Known for its anti-inflammatory properties and ability to help regulate oil production and support the skin barrier. Often found in serums and moisturizers.
3. Adjust Your Routine Pre-Period (Carefully!)
Anticipating the flare can help:
- Subtle Increase in Exfoliation: If your skin is well-acclimated and tolerant, you could add an extra application of your BHA or AHA exfoliant about 7-10 days before your expected period. Do not introduce new or harsh exfoliants during this sensitive time. Listen to your skin and back off if irritation occurs.
- Have Spot Treatments Ready: Keep your BPO or salicylic acid spot treatment handy to apply directly to any emerging blemishes as soon as you notice them.
- Consider Clay Masks: Using a clay mask once or twice in the week before your period can help absorb excess oil. Don’t overdo it, as excessive drying can backfire.
4. Lifestyle & Diet Considerations (Supportive Roles)
These factors influence overall hormonal balance and inflammation:
- Stress Management: High stress levels can exacerbate hormonal imbalances. Practice regular stress-reduction techniques like yoga, meditation, deep breathing, exercise, or spending time in nature.
- Diet Awareness: While highly individual, some women find reducing high-glycemic index foods (sugary snacks, refined carbs) and potentially dairy (if sensitive) in the week or two before their period may help lessen flare severity. Focus on whole foods and stay well-hydrated.
- Prioritize Sleep: Aim for 7-9 hours of quality sleep, as sleep deprivation affects hormone regulation and skin repair.
5. Hands Off! Avoid Picking or Squeezing
This is crucial, especially when dealing with inflamed hormonal breakouts. Picking worsens inflammation, spreads bacteria, and significantly increases the risk of scarring and persistent dark spots (PIH).
6. Consult a Dermatologist
If your cyclical breakouts are severe, cystic, painful, leave scars, or significantly impact your quality of life despite consistent OTC efforts, professional help is recommended.
Medical Treatments Specifically for Hormonal/Cyclical Acne
A dermatologist can offer targeted treatments that address the hormonal component:
- Oral Contraceptives: Certain combination birth control pills are FDA-approved to treat acne by regulating hormones.
- Spironolactone: An oral medication (originally a blood pressure drug) that blocks the effects of androgens on the skin’s oil glands. Highly effective for hormonal acne in women.
- Prescription Topical Retinoids: Stronger versions like Tretinoin.
- Other Prescription Topicals: Like clascoterone (Winlevi), which directly targets androgen receptors in the skin.
- Short-term Oral Antibiotics: Sometimes used to calm severe inflammatory flares.
- Isotretinoin (Accutane): Considered for severe, resistant nodulocystic acne, including hormonally influenced types.
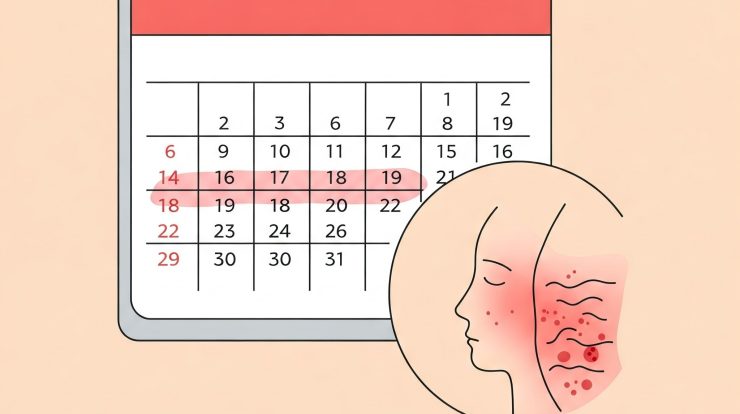
Patience and Tracking
Managing hormonal acne often requires patience. It can take 2-3 cycles to see if dietary or routine changes are making a difference. Tracking your menstrual cycle alongside your breakouts using a calendar or app can help you anticipate flares and tailor your preventative strategies more effectively.
Conclusion
Experiencing acne breakouts timed with your menstrual cycle is a common reality for many women due to underlying hormonal shifts. While completely preventing these flares can be challenging, a proactive and consistent management approach can significantly reduce their severity and impact. This involves maintaining a solid daily skincare routine year-round, strategically incorporating ingredients like salicylic acid or retinoids, making mindful pre-period adjustments, adopting supportive lifestyle habits, and resisting the urge to pick. For persistent, severe, or scarring cyclical acne, consulting a board-certified dermatologist is the most effective path towards finding targeted medical treatments that address the hormonal drivers.
