Not all “breakouts” are created equal. If you’re dealing with persistent skin bumps, understanding their true nature is the first critical step towards effective treatment. Two conditions often confused, yet requiring vastly different approaches, are cystic acne (a severe form of acne vulgaris) and “fungal acne” (more accurately known as Malassezia folliculitis or Pityrosporum folliculitis). While both can cause distress, they stem from different culprits and thus respond to different therapies. This article will highlight the key differences between cystic acne and fungal acne to help you better understand what might be happening with your skin.
Important Disclaimer: This information is for educational purposes to help you understand potential differences. Self-diagnosis can be misleading and delay appropriate care. Always consult a board-certified dermatologist for an accurate diagnosis and personalized treatment plan.
What is Cystic Acne?
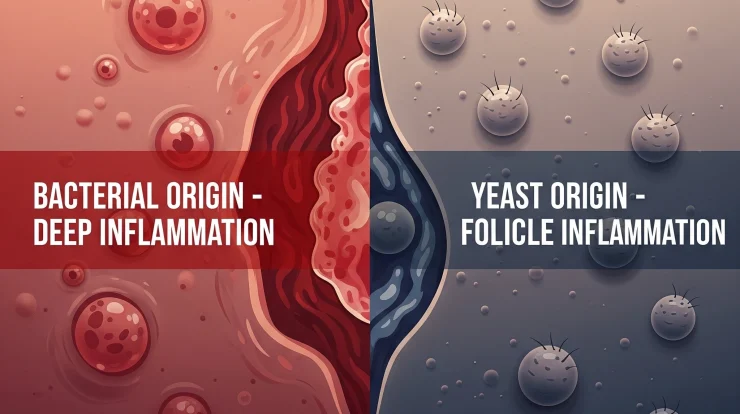
Cystic acne is a severe, inflammatory type of acne vulgaris, which is primarily caused by a combination of factors:
- Cause:
- Excess Sebum (Oil) Production: Often influenced by hormones (androgens).
- Clogged Pores: Dead skin cells mix with sebum, blocking hair follicles.
- Bacteria: Overgrowth of Cutibacterium acnes (formerly Propionibacterium acnes) bacteria within the clogged follicle.
- Deep Inflammation: The body’s immune response to the bacteria and clogged follicle leads to significant inflammation deep within the dermis.
- Appearance:
- Characterized by large, deep, painful, and often tender cysts and nodules under the skin.
- These lesions can be pus-filled or hard to the touch.
- They are typically varied in size and shape and can take weeks or even months to resolve.
- Common Locations: Most common on the face (especially jawline, chin, and cheeks in hormonal patterns), but can also occur on the chest, back, shoulders, and neck.
- Itchiness: Generally, cystic acne lesions are more painful or tender than itchy, although some mild itchiness can occasionally occur with inflammation.
- Comedones (Blackheads/Whiteheads): Often, individuals with cystic acne will also have other forms of acne vulgaris, including blackheads and whiteheads, present on their skin.
- Scarring Risk: Very high. Due to the depth and severity of inflammation, cystic acne frequently leads to permanent scarring (indented or raised).
What is Fungal Acne (Malassezia Folliculitis)?
Despite its common name, “fungal acne” is not true acne. It’s an infection and inflammation of the hair follicles caused by an overgrowth of a type of yeast (a fungus) called Malassezia, which is naturally present on everyone’s skin.
- Cause:
- Overgrowth of Malassezia Yeast: This yeast normally lives harmoniously on the skin, but certain conditions can cause it to multiply excessively and irritate hair follicles.
- Appearance:
- Typically presents as small, uniform, often monomorphic (similar-looking) papules and pustules, usually 1-2mm in size.
- These bumps can look like a rash of tiny pimples and may sometimes have a small whitehead.
- They often appear in clusters.
- Common Locations: Most frequently found on oily areas of the body where sweat accumulates, such as the chest, back, shoulders, and upper arms. It can also occur on the forehead, hairline, and sometimes the neck or jawline, especially in humid climates like Indonesia.
- Itchiness: A key distinguishing feature – fungal acne is often very itchy, especially when the skin is warm or sweaty.
- Comedones (Blackheads/Whiteheads): Typically absent or rare in areas solely affected by fungal acne. If comedones are present, it might indicate co-existing acne vulgaris.
- Triggers:
- Hot, humid environments (sweat creates a favorable environment for yeast).
- Tight, occlusive clothing that traps moisture and heat.
- Oily skin.
- Prolonged use of broad-spectrum antibiotics (which can disrupt the skin’s bacterial balance, allowing yeast to overgrow).
- Immunosuppression.
- Sometimes, use of oily or occlusive skincare products that can feed the yeast.
Key Differences Summarized
Why Correct Diagnosis Matters Immensely
Understanding the difference is critical because the treatments are completely different:
- Misdiagnosis Delays Relief: Using treatments for bacterial acne on fungal acne will be ineffective and can be frustrating.
- Potential to Worsen: Crucially, using antibiotics (oral or topical) for suspected acne can actually make fungal acne worse by further disrupting the skin’s natural microbiome and allowing the Malassezia yeast to flourish even more.
- Preventing Scarring: For cystic acne, delaying appropriate medical treatment significantly increases the risk of permanent scarring.
How a Dermatologist Diagnoses the Difference
A board-certified dermatologist is best equipped to differentiate between these conditions:
- Visual Examination: The appearance, location, and distribution of the lesions provide important clues.
- Patient History: Information about itchiness, triggers (like humidity or antibiotic use), and response to previous treatments is vital.
- Skin Scraping & Microscopy: For suspected fungal acne, a dermatologist may gently scrape some skin cells from an affected area to examine under a microscope for the presence of Malassezia yeast.
- Wood’s Lamp Examination: Malassezia yeast can sometimes fluoresce a yellowish-green color under a Wood’s lamp (a type of black light).
- Fungal Culture or Biopsy: In some unclear or resistant cases.
Contrasting Treatment Approaches
- Cystic Acne Treatment: Typically involves a combination of approaches prescribed by a dermatologist, such as:
- Topical retinoids (e.g., tretinoin, adapalene)
- Benzoyl peroxide
- Topical and/or oral antibiotics (to reduce bacteria and inflammation)
- Hormonal therapies (for women, e.g., birth control pills, spironolactone)
- Oral isotretinoin (for severe, resistant cases)
- Cortisone injections (for individual large cysts)
- Fungal Acne (Malassezia Folliculitis) Treatment: Focuses on reducing the yeast overgrowth:
- Topical Antifungal Washes/Shampoos: Products containing ketoconazole (e.g., Nizoral shampoo), selenium sulfide (e.g., Selsun Blue shampoo), or pyrithione zinc used as a body/face wash on affected areas (lather and leave on for 5-10 minutes before rinsing).
- Topical Antifungal Creams: Clotrimazole, miconazole, or ketoconazole creams.
- Oral Antifungal Medications: For widespread or resistant cases, a dermatologist might prescribe short courses of oral antifungals like fluconazole or itraconazole.
- Lifestyle Adjustments: Wearing loose, breathable clothing, showering promptly after sweating, and sometimes adjusting skincare to avoid heavy oils that might feed the yeast.
Conclusion
While both cystic acne and fungal acne (Malassezia folliculitis) can cause distressing skin breakouts, they are fundamentally different conditions driven by different microorganisms and requiring distinct treatment strategies. Key differentiating factors often include the appearance of the lesions (large, varied, and painful cysts vs. small, uniform, and itchy bumps), the presence or absence of comedones, and the primary locations affected.
Self-diagnosing can be challenging and potentially lead to ineffective or even counterproductive treatments. If you are experiencing persistent, itchy, or unusual breakouts, especially on your chest, back, shoulders, or forehead, it is crucial to consult a board-certified dermatologist. They can provide an accurate diagnosis and recommend the most appropriate and effective treatment plan to help you achieve clearer, more comfortable skin.
