Acne is a common skin condition with a variety of underlying causes and contributing factors. When trying to understand and treat breakouts, you might encounter terms like “hormonal acne” and “bacterial acne.” While these terms are often used, their relationship can be nuanced and sometimes confusing, as they aren’t always mutually exclusive. Understanding the primary drivers and typical characteristics associated with these descriptions is key to seeking the most effective treatment.
This article aims to clarify the distinctions and overlaps between what is commonly referred to as hormonal acne and the role of bacteria in acne development.
Important Disclaimer: Acne is a complex medical condition. This information is for educational purposes and should not be used for self-diagnosis. Always consult a board-certified dermatologist for an accurate diagnosis and a personalized treatment plan.
What is Hormonal Acne?
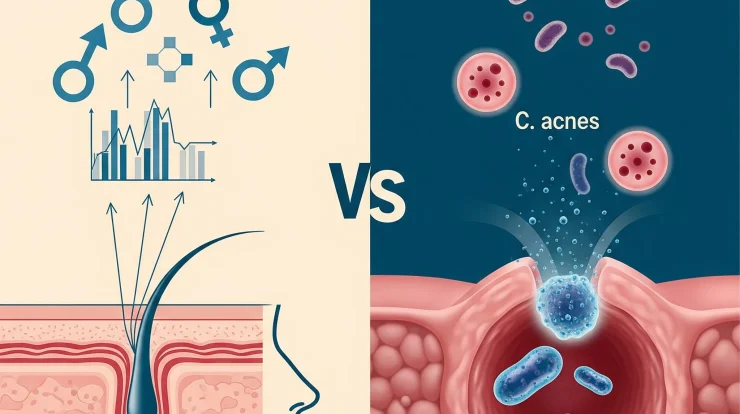
Hormonal acne is acne that is primarily driven or significantly exacerbated by fluctuations or imbalances in hormones.
- Primary Driver: The main culprits are androgens (such as testosterone and dihydrotestosterone – DHT), which are present in both men and women. These hormones stimulate the skin’s sebaceous (oil) glands to produce more sebum. In women, the cyclical interplay of estrogen and progesterone throughout the menstrual cycle, and their ratio to androgens, also significantly influences skin behavior. Furthermore, hormones like insulin and Insulin-like Growth Factor 1 (IGF-1) can indirectly boost androgen production or sensitivity.
- Mechanism: Excess sebum, combined with an abnormal shedding of skin cells (keratinocytes) within the hair follicle, leads to clogged pores (comedones). This environment then becomes conducive to the proliferation of Cutibacterium acnes bacteria, triggering inflammation.
- Typical Symptoms/Patterns:
- Location: Classically appears on the lower third of the face – the jawline, chin, around the mouth, and often the neck. It can also occur on the chest and back.
- Timing (especially in women): Often exhibits a cyclical pattern, with flare-ups occurring predictably in the week(s) leading up to or during menstruation. It can also be persistent in adulthood (adult-onset acne).
- Lesion Type: Tends to be more inflammatory and deeper, such as tender papules (red bumps), pustules (pimples with pus), and often more severe nodules or cysts (large, painful, under-the-skin lesions).
- Persistence: Can be stubborn and may not respond as readily to simple topical treatments alone.
- Other Hormonal Signs: In some women, it may be accompanied by other signs of hormonal imbalance like irregular periods or hirsutism (excess facial/body hair), as seen in conditions like Polycystic Ovary Syndrome (PCOS).
What is Meant by “Bacterial Acne”?
The term “bacterial acne” is often used to describe the inflammatory aspect of acne vulgaris where the bacterium Cutibacterium acnes (formerly Propionibacterium acnes or P. acnes) plays a key role.
- Role of Bacteria: C. acnes is a bacterium that normally lives on most people’s skin, often harmlessly within hair follicles. It’s not typically about external bacterial contamination causing acne in the way a skin infection might occur.
- Mechanism: When a hair follicle becomes clogged with excess sebum and dead skin cells (forming a microcomedone), an anaerobic (low-oxygen) environment is created. C. acnes thrives in these conditions and proliferates. As the bacteria multiply, they release enzymes and byproducts that trigger an immune response from the body, leading to inflammation. This inflammation manifests as the redness, swelling, pain, and pus characteristic of pimples, pustules, nodules, and cysts.
- “Bacterial Acne” as a Descriptive Term: It’s crucial to understand that virtually all inflammatory acne lesions, including those in hormonally-driven acne, have a bacterial component contributing to the inflammation. The term “bacterial acne” isn’t a distinct scientific category separate from common acne vulgaris in the same way that a “hormonal pattern” of acne is described. It might be used loosely to refer to:
- Acne where the inflammatory, bacteria-driven aspect seems particularly dominant and visible.
- Acne that shows a good initial response to treatments targeting bacteria (like benzoyl peroxide or antibiotics).
- Sometimes, very localized breakouts potentially triggered by external bacterial transfer (e.g., from a dirty phone or helmet), though this is less about the systemic nature of acne vulgaris.
Hormonal Acne vs. Bacterial Acne: Key Distinctions & Overlaps
The core difference lies in the primary driving force or instigator, although the processes are interconnected:
Why Understanding the Primary Driver Matters for Treatment
Recognizing whether hormonal influences are a dominant factor in your acne is crucial for effective long-term management:
- Targeted Treatment: If significant hormonal drivers are present, treatments that only address surface bacteria or mild pore clogging (like some basic OTC products) may provide limited or temporary relief. More targeted therapies that influence hormone activity or its effects on the skin are often needed.
- Avoiding Antibiotic Overuse: If acne is primarily hormonally driven, long-term reliance solely on antibiotics (oral or topical) without addressing the hormonal component can lead to antibiotic resistance and diminishing effectiveness.
- Managing Expectations: Understanding the root cause helps set realistic expectations for treatment timelines and outcomes.
The Role of a Dermatologist
A board-certified dermatologist plays an essential role in:
- Accurate Diagnosis: They consider your medical history (including menstrual history for women), family history, the appearance and distribution of your acne lesions, and your response to previous treatments. Sometimes, blood tests to check hormone levels may be indicated if PCOS or another hormonal disorder is suspected.
- Creating a Tailored Treatment Plan: Based on the diagnosis, they can devise a comprehensive treatment strategy that addresses the primary drivers of your specific acne, whether it’s predominantly hormonal, highly inflammatory due to bacterial activity, or a combination.
Conclusion
The terms “hormonal acne” and “bacterial acne” can sometimes cause confusion because they are not entirely separate entities. All common inflammatory acne involves the bacteria C. acnes contributing to inflammation. However, hormonal acne specifically refers to acne where internal hormonal fluctuations or imbalances are the primary trigger that sets the stage for breakouts – typically by increasing oil production, which then allows bacteria to thrive in clogged pores.
Recognizing patterns suggestive of hormonal influence – such as breakouts on the jawline and chin, cyclical flares in women, or persistent adult acne that’s often deep and inflammatory – is an important step. This understanding helps guide treatment towards addressing these internal drivers, often alongside strategies to manage bacteria and inflammation on the skin’s surface. Ultimately, for persistent or severe acne, a consultation with a dermatologist is paramount to receive an accurate diagnosis and a multi-faceted treatment plan that effectively targets all contributing factors for your specific condition.
